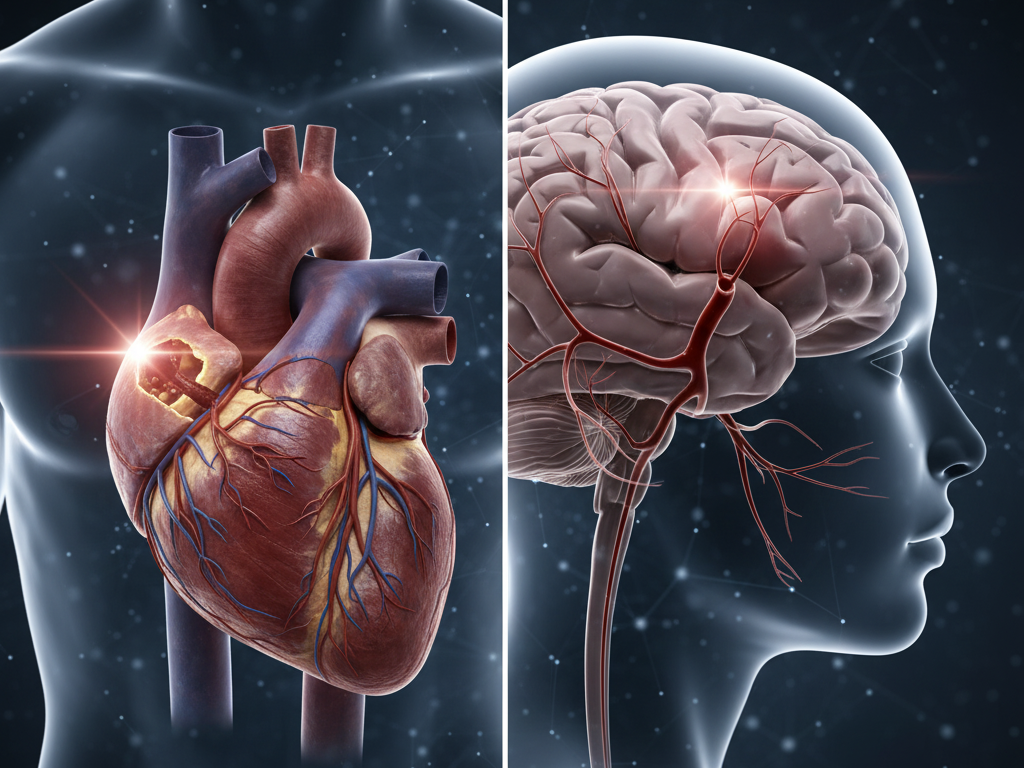
In the realm of cardiovascular crises, few events are as sudden, terrifying, and potentially fatal as a heart attack or a stroke. Both conditions involve a rapid disruption of blood flow, often share similar risk factors, and require immediate emergency intervention. For these reasons, they are frequently confused, leading to delays in crucial treatment.
Understanding the fundamental key differences between a heart attack (Myocardial Infarction) and a stroke (Cerebrovascular Accident) is more than just academic knowledge—it is truly lifesaving knowledge. While both are considered cardiovascular events, they affect different organs and present with unique symptoms, demanding distinct medical responses. Knowing which organ is under attack determines the specific treatment path and dramatically influences the patient’s chances of recovery.
This comprehensive guide will demystify these two major health threats. We will dive deep into the specific causes, contrasting symptoms, and the shared prevention strategies that can protect your vital organs. Empower yourself with the knowledge to recognize, differentiate, and potentially prevent these two leading causes of global morbidity and mortality.
The Core Distinction: Organ Under Attack
The most fundamental key difference between a heart attack and a stroke lies in the organ that suffers the critical loss of oxygen and nutrients. Both are typically caused by a blockage, but where that blockage occurs defines the crisis.
The Heart Attack: A Plumbing Problem in the Cardiac Muscle
A heart attack occurs when blood flow to the heart muscle itself is severely reduced or completely blocked. This blockage is most commonly caused by a rupture of plaque (atherosclerosis) within the coronary arteries, which supply oxygen-rich blood to the heart. When the heart muscle is starved of oxygen, it begins to die, leading to the infarction.
The primary mechanism is a circulatory failure localized to the heart. The severity of the damage depends on the size of the artery blocked and the duration of the lack of blood flow. Timely medical intervention is essential to restore blood flow and save the cardiac tissue.
The Stroke: A Blockage or Bleed in the Brain
A stroke occurs when blood flow to a specific area of the brain is suddenly interrupted. Since brain cells begin to die within minutes without oxygen, a stroke is a true neurological emergency. Strokes are categorized into two main types:
- Ischemic Stroke (87% of cases): This type is caused by a blockage—a blood clot that travels to or forms in an artery supplying the brain. This is similar to the cause of a heart attack but occurs in the brain’s circulation.
- Hemorrhagic Stroke (13% of cases): This type is caused by a blood vessel rupturing and bleeding into the brain tissue, leading to swelling and damaging brain cells.
The location of the stroke determines the specific symptoms and the resulting neurological deficits, as different parts of the brain control different bodily functions.
Symptoms and Warning Signs: How to Differentiate the Crisis
While both are life-threatening emergencies, the symptoms of a heart attack are typically focused on the chest and upper body, while the symptoms of a stroke are primarily neurological and focus on the face, limbs, and speech. Recognizing these key differences allows for quicker emergency response and better patient outcomes.
The Symptoms of a Heart Attack
A heart attack often presents as crushing chest pain, but the symptoms can be varied and, crucially, may be very different for men and women.
- Classic Chest Pain (Angina): Discomfort, pressure, squeezing, fullness, or pain in the center of the chest that lasts more than a few minutes, or goes away and comes back. This is the most common symptom.
- Upper Body Discomfort: Pain or discomfort radiating to one or both arms (often the left), the back, neck, jaw, or stomach.
- Shortness of Breath: This may occur before or accompany the chest discomfort.
- Other Symptoms (More Common in Women):
- Unusual fatigue that lasts for days.
- Nausea, vomiting, or lightheadedness.
- Cold sweat or clamminess.
Note: If you suspect a heart attack, call emergency services immediately. Do not attempt to drive yourself or the patient to the hospital.
The Symptoms of a Stroke: Recognizing F.A.S.T.
The most widely taught, effective method for spotting a stroke is the F.A.S.T. acronym. Time is brain, and immediate recognition is paramount for utilizing clot-busting drugs (thrombolytics) which must be administered within a specific, short time window.
- F – Face Drooping: Ask the person to smile. Does one side of the face droop or feel numb?
- A – Arm Weakness: Ask the person to raise both arms. Does one arm drift downward? Is one arm weak or numb?
- S – Speech Difficulty: Ask the person to repeat a simple phrase. Is their speech slurred, strange, or difficult to understand? Are they unable to speak?
- T – Time to Call 911 (or local emergency services): If any of these symptoms are present, even if they disappear, call immediately. Note the time the first symptom appeared.
Other stroke symptoms may include sudden severe headache, sudden trouble seeing in one or both eyes, sudden trouble walking, dizziness, or loss of balance.
Shared Causes and Common Risk Factors
Despite their distinct locations and manifestations, heart attack and stroke are fundamentally diseases of the vascular system. This means they share the same major risk factors and prevention strategies. Addressing these underlying issues is the key to long-term health.
The Primary Cause: Atherosclerosis
The vast majority of both heart attack (blockage of coronary arteries) and ischemic stroke (blockage of cerebral arteries) are rooted in atherosclerosis—the buildup of fatty plaque inside the artery walls. This plaque narrows the vessels, making them stiff and restricting blood flow. When the plaque ruptures, it forms a clot that can completely block the artery, triggering the event.
Key Risk Factors Common to Both
For those seeking to reduce their cardiovascular risk, focusing on the following modifiable risk factors is essential for prevention.
| Risk Factor | Impact on Cardiovascular Health | Prevention Strategy |
| High Blood Pressure (Hypertension) | Damages and stiffens arteries, making them prone to plaque rupture and clotting in both the heart and brain. | Healthy eating (DASH diet), sodium reduction, and consistent medication. |
| High Cholesterol | Leads directly to the buildup of fatty plaque in artery walls (atherosclerosis). | Limit saturated and trans fats; increase soluble fiber and omega-3s. |
| Diabetes | High blood sugar levels damage blood vessel walls, greatly accelerating atherosclerosis and increasing the risk of clots. | Strict blood sugar control through diet, physical exercise, and medication. |
| Obesity | Increases the workload on the heart and is linked to high blood pressure, diabetes, and high cholesterol. | Weight loss through balanced healthy eating and routine physical exercise. |
| Smoking | Chemicals damage the lining of blood vessels, accelerate plaque growth, and thicken the blood, increasing the risk of clot formation. | Cessation is the single most important preventative action. |
| Physical Inactivity | Contributes to high blood pressure, obesity, and poor circulation. | Aim for 150 minutes of moderate physical exercise per week. |
Prevention and Recovery: Long-Term Health Strategies
Since the underlying causes are shared, the prevention strategies for heart attack and stroke are virtually identical, focusing on comprehensive lifestyle changes to achieve optimal health.
Primary Prevention: The Lifestyle Foundation
The most effective tool against both cardiovascular events is a commitment to a healthy lifestyle.
- Adopt a Heart-Healthy Diet: Emphasize the DASH (Dietary Approaches to Stop Hypertension) or the Mediterranean diet. These focus on whole grains, fruits, vegetables, lean protein, and healthy fats while drastically limiting sodium and red meat. This supports weight loss and blood pressure control.
- Maintain a Healthy Weight: Losing excess body fat reduces the strain on your heart and lowers blood pressure levels. Even a modest weight loss of 5-10% can significantly lower cardiovascular risk.
- Exercise Regularly: Engage in routine physical exercise (e.g., brisk walking, swimming) for at least 30 minutes, most days of the week. Exercise strengthens the heart and makes blood vessels more flexible.
- Manage Chronic Conditions: Work closely with your physician to keep blood pressure, cholesterol, and blood sugar levels within recommended target ranges through medication and monitoring.
The Road to Recovery: Rehabilitation
Recovery after both a heart attack and a stroke involves specialized rehabilitation, although the focus differs significantly based on the damaged organ.
- Heart Attack Recovery (Cardiac Rehab): Focuses on restoring the heart’s function. This involves monitored physical exercise, nutritional counseling, emotional support, and intensive patient education on medication management. The goal is to strengthen the remaining heart muscle and prevent future events.
- Stroke Recovery (Neurological Rehab): Focuses on regaining lost neurological function. This involves physical therapy (to regain movement), occupational therapy (to relearn daily tasks), and speech therapy (to regain communication skills). The brain’s plasticity allows healthy areas to take over functions from damaged areas, making intensive early rehab critical for meaningful recovery.
Frequently Asked Questions (FAQ)
Is a “mini-stroke” the same as a TIA?
Yes. A Transient Ischemic Attack (TIA) is often called a “mini-stroke.” It is caused by a temporary blockage of blood flow to the brain, causing stroke-like symptoms that typically last less than 24 hours (often just a few minutes) and cause no permanent damage. However, a TIA is a major warning sign that a full stroke may follow soon, and requires immediate medical evaluation and aggressive prevention strategies.
Does a heart attack always involve chest pain?
No. While severe chest pain is the classic symptom, a significant number of heart attacks—particularly in women, older adults, and individuals with diabetes—can be “silent” or present with atypical symptoms like profound fatigue, nausea, shortness of breath, or discomfort only in the jaw or back. This highlights why regular health screenings are so important.
How are the two crises treated differently in the emergency room?
The initial goal for both is restoring blood flow, but the treatments are organ-specific:
- Heart Attack: Treatment often involves catheterization procedures (angioplasty and stenting) to physically open the blocked coronary arteries and administer anti-clotting drugs.
- Stroke: For an ischemic stroke, treatment involves administering clot-busting drugs (thrombolytics) within a critical 3-4.5 hour window, or performing mechanical thrombectomy (removing the clot) for large vessel blockages. Hemorrhagic strokes require surgery to control the bleeding and relieve pressure.
Conclusion
Both the heart attack and the stroke are urgent cardiovascular events demanding immediate recognition and specialized care. While a heart attack attacks the heart muscle, a stroke attacks the brain. Knowing the key differences—especially the neurological symptoms (F.A.S.T.) of a stroke versus the chest/upper body symptoms of a heart attack—is crucial for ensuring rapid emergency response and increasing the chances of full recovery.
Crucially, both crises share common ground: they are largely preventable. By controlling blood pressure, managing weight loss, adopting healthy eating habits, and committing to regular physical exercise, you can drastically reduce your cardiovascular risk and secure your long-term health.
Ready to take control of your cardiovascular risk? Schedule your next blood pressure and cholesterol screening today, and check out our guides on the DASH diet and effective physical exercise routines to start building your foundation for optimal health!

Leave a comment